Osteoporosis
What is osteoporosis?
Osteoporosis is a loss of bone when compared to peak bone mass resulting in increased bone fragility. Osteopenia is also a loss of bone, but not as severe as osteoporosis. Our practice treats both osteopenia and osteoporosis and the diagnostic steps, laboratory workups, and treatments strategies are fairly similar with the exception that the treatment for osteoporosis tends to be more aggressive than that of osteopenia.
Who is affected by osteoporosis?
Anyone can be affected as we mature, although it seems to be slightly more common in post-menopausal women than in men. This may be due to the fact that women are naturally smaller than men and also more likely to be screened than men. People taking certain medications that can exacerbate bone loss are also at increased risk for osteoporosis.
Why do we treat osteoporosis?
We treat osteoporosis because the diagnosis implies that bone strength has been diminished resulting in increased bone fragility and more brittle bones. Patients with osteoporosis are at a higher risk for bone fractures or breaks which can lead to further health issues.
What causes osteoporosis?
The most common cause of osteoporosis is due to the hormonal changes associated with menopause, and in men, andropause. However, our practice regularly screens patients for other causes of osteoporosis including vitamin and mineral deficiencies, malabsorption problems, hormonal abnormalities related to the thyroid, parathyroid, or adrenals, and liver and kidney issues. We also screen for other causes such as blood disorders, and the use of certain medications or substances that can increase the risk for developing osteoporosis.
How is osteoporosis diagnosed?
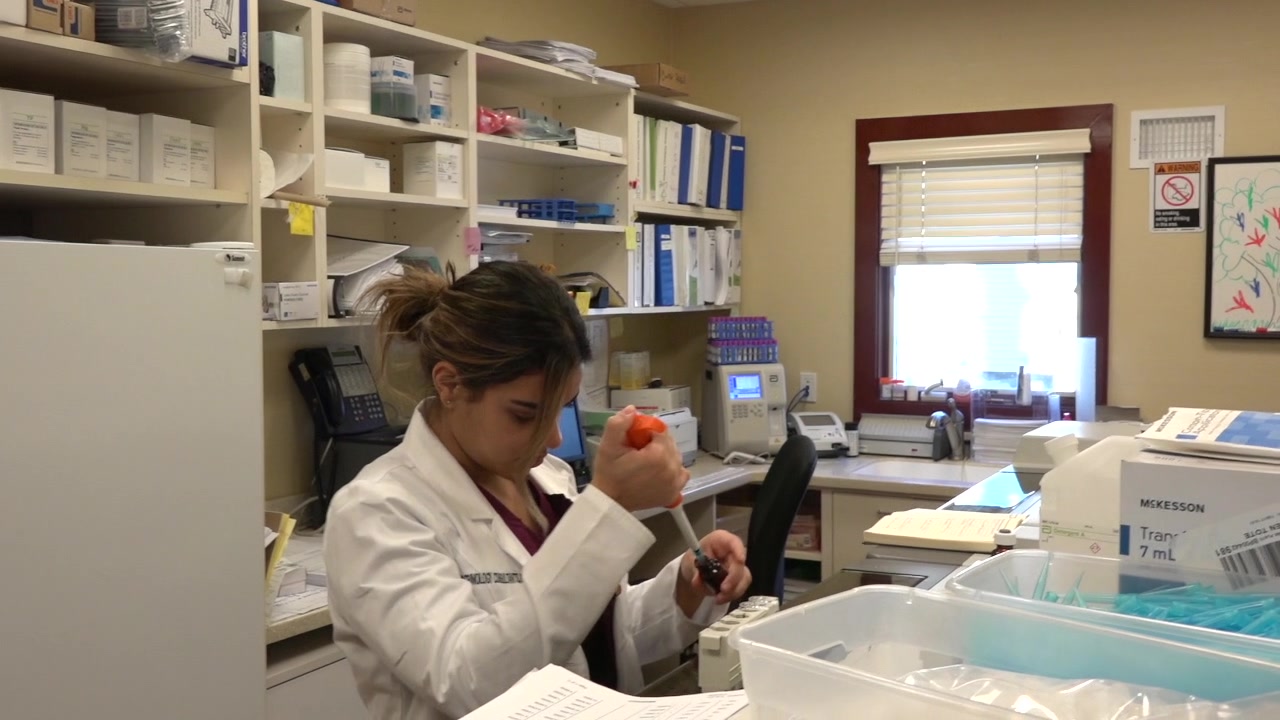
Osteoporosis is diagnosed with the use of a bone density DEXA scan (dual-energy x-ray absorptiometry) and our facility is equipped with a state of the art bone density machine.
How is osteoporosis treated?
First, our practiced professional’s screen for secondary causes of osteoporosis using blood and urine studies. If any causes are identified, we address those issues first, either here in our office or with referrals to respected colleagues. Once the secondary causes have been addressed, we confirm that patients are getting appropriate amounts of vitamins and minerals through supplementation or dietary intake. Our practice places a strong emphasis on lifestyle modification, with the incorporation of specific exercises to stimulate bone build up and growth. Lastly, we explain the various types of bone-sparing medications (medications that decrease fracture rate) and find the most suitable medication for each patient. We continue to monitor a patient’s response to the various interventions both with regular laboratory workups as well as bone density assessments.